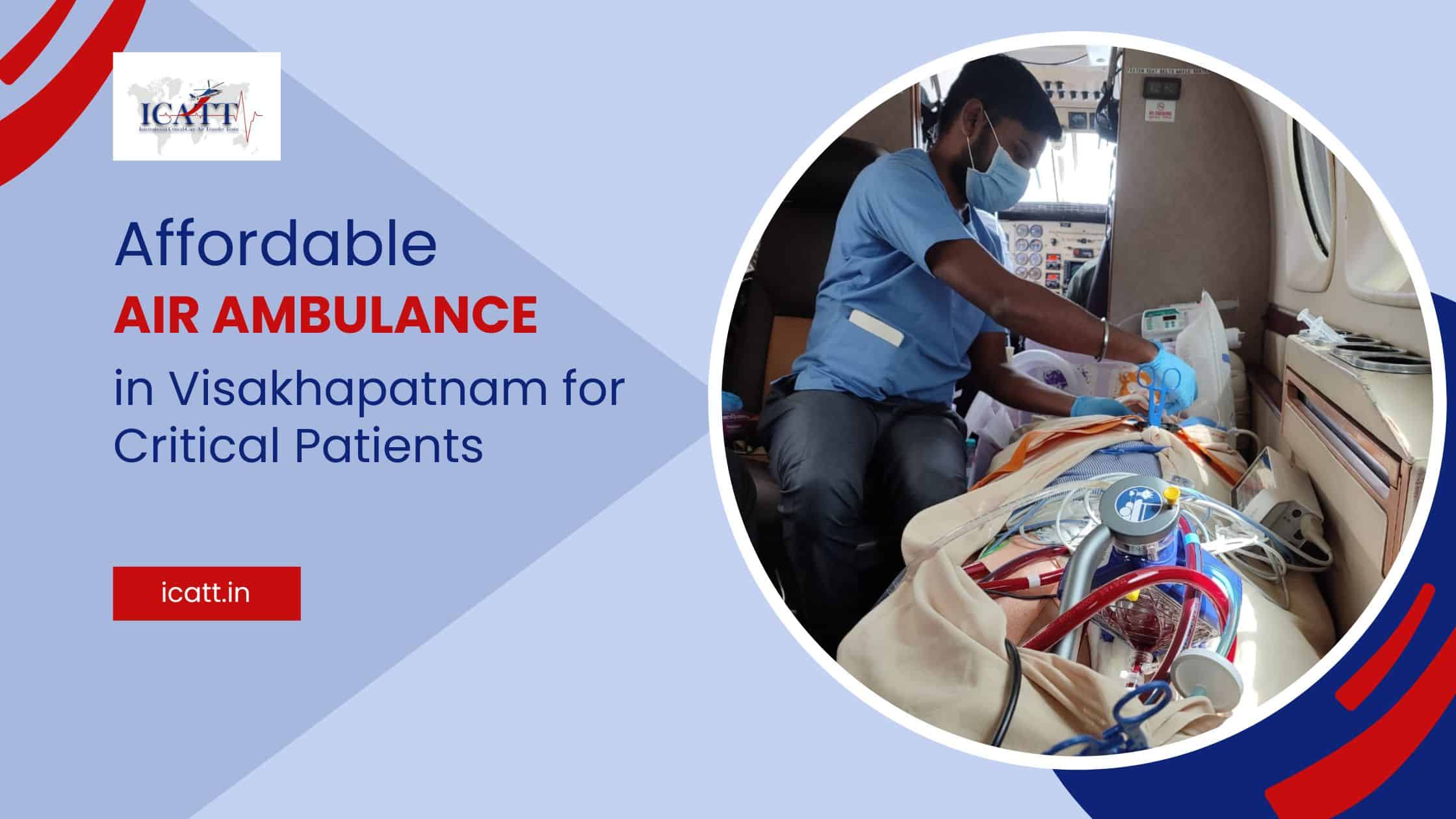
Extracorporeal membrane oxygenation or ECMO machine replaces the function of the heart and lungs. ECMO helps some patients for whom a mechanical ventilator alone is not sufficient to breathe safely.
Like the cardiopulmonary devices commonly used in open-heart surgery, the ECMO pumps and delivers oxygen to the patient’s blood. Conversely, patients sometimes stay on ECMO for days to allow their bodies to recover from life-threatening conditions, including COVID-19.
According to ICATT, using life support machines like ECMO to replicate the heart and lung function has significantly improved the survival rate of outpatient heart attacks. The treatment program, which includes a life support machine called extracorporeal membrane oxygenation (ECMO), was much more effective than standard treatment for this often fatal condition.
Let us know more about the Survival rate of patient transport with ICATT’s ECMO services.
What is ECMO?

ECMO stands for Extracorporeal Membrane Oxygenation. It is also referred to as ECLS or extracorporeal Life Support. ECMO is a special machine that does the work of the heart and lungs. ECMO allows the heart or lungs to rest and heal. ECMO does not treat these organs but functions on behalf of these vital organs.
ECMO is very similar to an open heart surgical machine. However, patients are put on open-heart surgical machines for hours, while on ECMO, they are there for days to weeks.
When is the ventilator not enough?
Most patients treated with ECMO were already ventilated. However, ECMO is used if the ventilator itself does not meet the patient’s needs.
Usually, the lungs take in oxygen and emit CO2. But if the ventilator can no longer provide this support or the pressure itself can cause damage, ECMO can help.
Prolonged pressure of ventilator support on the lungs can lead to lung injury; in extreme circumstances. Pneumothorax is a potentially lethal complication associated with mechanical ventilation. Most of the patients with pneumothorax from mechanical ventilation have underlying lung diseases; pneumothorax is rare in intubated patients with normal lungs. Tension pneumothorax is more common in ventilated patients with prompt recognition and treatment of pneumothorax being important to minimize morbidity and mortality. Underlying lung diseases are associated with ventilator-related pneumothorax with pneumothoraces occurring most commonly during the early phase of mechanical ventilation
When ECMO exchanges oxygen and carbon dioxide, less pressure is required in the ventilator. This allows the patient’s body to heal, while the medical team can use drugs and other treatments to speed up the healing.
What is the purpose of ECMO?

By taking over the work of the “diseased” heart or the lungs – ECMO gives these organs time to rest and heal. ECMO does not deal with organs. It just gives them a break. ECMO is only used after all other medical measures have been tried. When the heart or lungs recover, the patient is taken off ECMO. This can take days to weeks in adult patients.
How does ECMO work?
Cannulas are placed in the arteries or veins of the patient’s neck and groin. They can be placed surgically or percutaneously. This means they will be placed as an IV. The ECMO doctor will determine which method is required. This cannula allows blood to be drawn from the patient and travel through the ECMO chain, where oxygen is added and carbon dioxide is removed. It is then warmed and returned to the patient via the second cannula. At this point, all adult ECMO patients will need 2 ECMO cannulas.
ECMO type

The ECMO circuit can be adjusted in three ways:
- Venous Arterial ECMO (VA-ECMO): Allows gas exchange and hemodynamic support while pumping blood from a vein to the side of the artery. This system supports the heart and lungs like the systems used in cardiac surgery operating rooms.
- Venous-venous (VV-ECMO): Facilitates gas exchange. The blood is drained from the side of the vein and then pumped back in. This system supports only the lungs.
- Arterial-Venous ECMO (AV-ECMO): Facilitates gas exchange by using the patient’s blood pressure to pump blood from the artery to the side of the vein.
The circuit arrangements for VA or VV are almost identical. The movement of blood is facilitated by an external pump. The pump pushes the blood through the membrane allowing for gas exchange (oxygen and CO2 removal) before the blood is returned to the patient’s circulation by heating.
Due to its configuration, the VA-ECMO passes through the patient’s heart and lungs and part or all of the blood flow is diverted through the ECMO chain. In contrast, VV-ECMO returns blood before it enters the pulmonary circulation.
When incorporeal circulation (AV-ECMO) is used, blood flows from the femoral artery through the membrane and passively returns to the femoral vein. The whole process depends on the volume of the patient’s heart.
The ECMO doctor decides during cannulation which method is best.
Clinical indications for ECMO support
ECMO is used in patients with refractory cardiogenic shock who have potentially severe reversible heart disease. However, it can also be used as a bridge to a ventricular assist device (VAD) or a heart transplant. VA-ECMO can also be used as a rescue technique during a heart attack. Current data support their use after unsuccessful 10 minutes of Life Support Extension (ALS).
The survival rate of patients transported using ICATT’s ECMO service

Survival for patients with ICATT’s ECMO varies between 30% and 50%, depending on the cause of the cardiac dysfunction. ECMO can be considered in patients with systolic blood pressure below 85 mm Hg. If the cardiac index is below 1.2-litre min/m2 despite sufficient preload, more than two inotropes are used, intra-aortic balloon counterpulsation (IABP) and signs of low systemic levels of cardiac output.
This is one of the most expensive therapies in the intensive care unit. The following multidisciplinary team members are involved:
- ECMO is the attending physician.
- Critical care physician.
- Pulmonary specialist.
- Cardiac specialist.
- Nurse practitioner.
- Critical care bedside nurses.
- Respiratory therapist.
- Pharmacist.
- Physical and occupational therapists.
- Psychology, psychiatry and spiritual care providers.
- Child life specialist for pediatric patients.
Conclusion:
As outlined in detail above, ECMO is for those patients who have acute heart and lung problems. Upon successful transport of patients to the nearest multispeciality hospital, treatment can be continued by the doctors. Transport of patients with ECMO support is safe and should be carried out under the able guidance of an ICATT trained team. For more information, contact ICATT Air ambulance at +91-9701111156.